By Josh Gray and Holli White
Background
Academic medical centers have a highly complex agenda: maintaining clinical excellence, pursuing cutting edge research, promoting medical education, and maintaining financial viability. As the country evolves towards value-based incentive care, is it realistic to expect AMCs to excel at population health as well? Josh Gray, Vice President of Analytic Services, and Stewart Richardson, Senior Data Scientist, recently completed an analysis of all MSSP and Medicare REACH ACOs for the first three quarters of 2023, using claims data from the CMS Virtual Research Data Center. Contact us to receive your ACO’s complimentary benchmarking report as well!
Analyzing the performance of Accountable Care Organizations (ACOs) sheds light on AMCs’ population health capabilities. ACOs are groups of physicians, hospitals, and other health care providers and business organizations that care for attributed patient populations, assuming responsibility for both clinical outcomes and the overall cost of care. Depending on their financial and quality performance, ACOs may either earn incentive payments or find themselves incurring financial penalties. Currently, about 11 million Medicare beneficiaries are attributed to ACOs through two of the Centers for Medicare and Medicaid Services’ (CMS) programs: the Medicare Shared Savings Program (MSSP) and the Realizing Equity, Access, and Community Health (REACH) program.
Of the roughly 456 MSSPs and 132 REACH ACOs that cared for Medicare fee-for-service beneficiaries in 2023, Health Data Analytics Institute (HDAI) estimates that 37 were closely affiliated with academic medical centers and cared for roughly 1.1 million attributed beneficiaries. We compared AMC cost effectiveness and proficiency in documenting care against the entire pool of CMS ACOs.
To compare cost-effectiveness across ACOs, we used HDAI’s Cost Savings Rate1, a proprietary indicator that compares the actual cost of all medical services for a given ACO with the cost of care for their digital twins. We also compared documentation practices across ACOs with our RAF Capture Rate2. RAF, or Risk Adjustment Factor, is a measure that captures the overall medical acuity of a given population and determines reimbursement levels for ACOs. ACOs that document their patient acuity more thoroughly have a higher RAF Capture Rate. ACOs with higher RAF Capture Rates tend to perform better financially, since ACO reimbursement is driven by the acuity of the patients they serve.
As indicated in the table below, ACOs affiliated with AMCs underperform financially relative to the entire pool of ACOs. For example, care costs for ACOs as a whole are 2.2% below expected levels, compared to 1.2% for ACOs affiliated with academic medical centers.
ACO performance
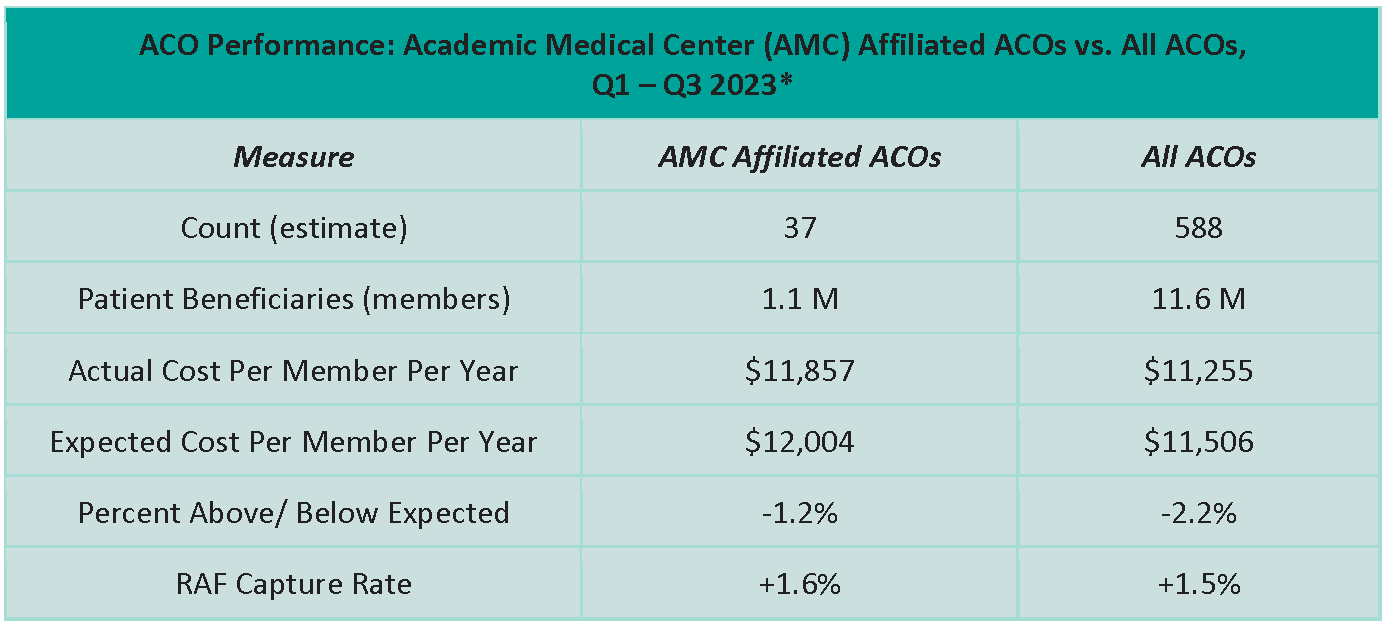
*Final numbers may change slightly due to claims lag.
Although ACOs affiliated with academic medical centers are less cost effective and less thorough in documenting acuity, a handful have achieved very high levels of performance, as indicated in the table below.
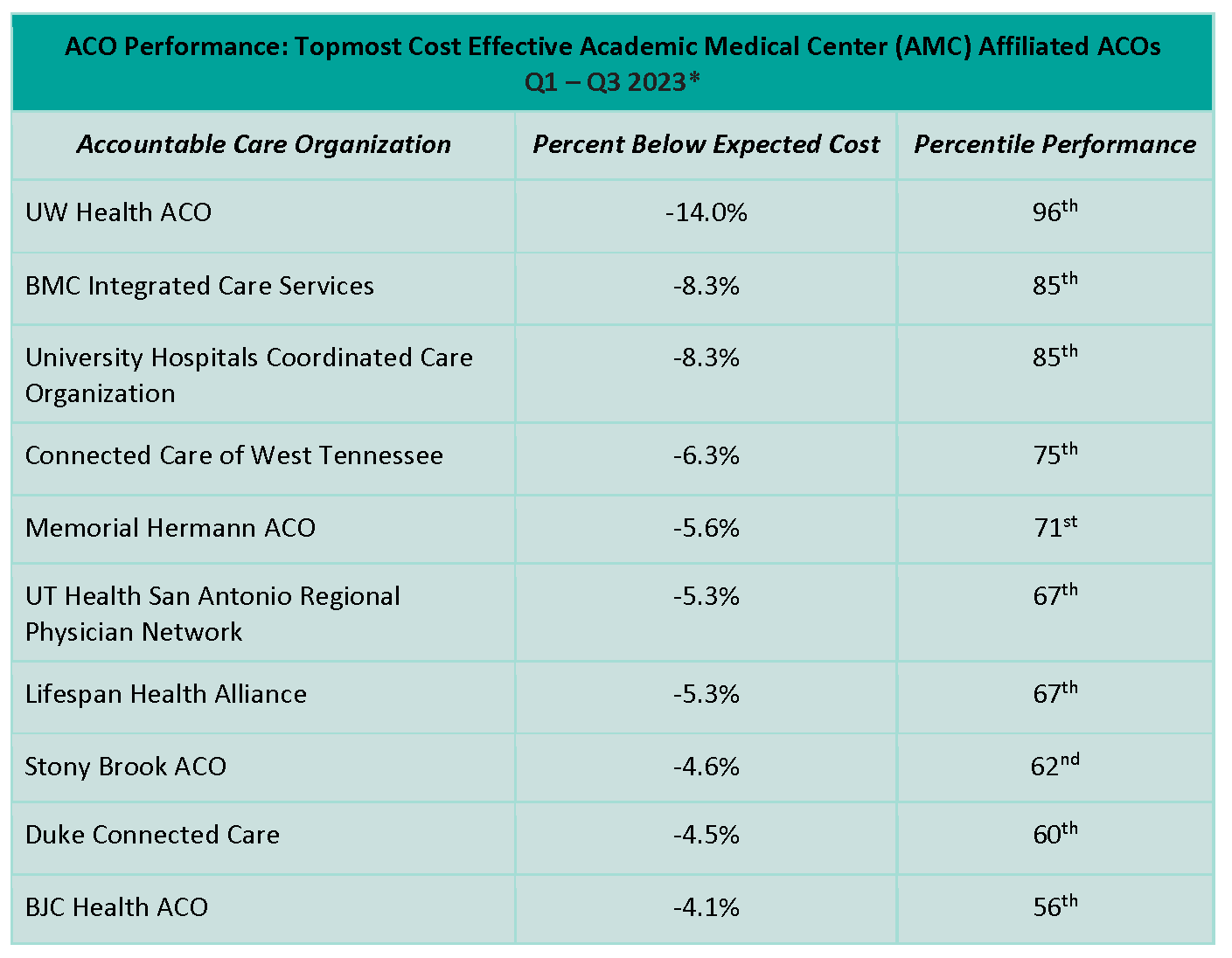
*Final numbers may change slightly due to claims lag.
This data indicates that although AMC-affiliated ACOs underperform ACOs as a whole, excellent performance is possible. For example, UW Health ACO in Wisconsin delivers cost savings of 14%, placing it in the 96th percentile for cost effectiveness among all ACOs. BMC Integrated Care Services in Boston and University Hospitals Coordinated Care Organization in Cleveland both place in the 85th percentile among all ACOs in terms of cost effectiveness. With the industry migrating towards value-based care, AMCs may leave themselves in a precarious position if they fail to develop strong capabilities in population health. The experience of leading academic ACOs indicates that providing cost effective care to a defined population is well within reach.
Contact us
If you work for an ACO affiliated with an academic medical center and have questions or suggestions about this analysis, we’d love to speak with you. Please email Josh at [email protected]. We would also be pleased to share a complimentary customized benchmarking report that will provide you with insight on your ACO’s performance relative to your peers.
Footnotes
1. HDAI Cost Savings Rate
HDAI’s Cost Savings Rate quantifies care costs for individual ACOs compared to all Medicare patients with similar demographics and medical histories. Every patient attributed to an ACO is matched to a set of digital twins selected from the roughly 30 million Medicare FFS beneficiaries in the CMS data set. Digital twins are precisely matched to each ACO beneficiary based on baseline clinical risk profile, location of patient residence, enrollment status, and recent medical services and procedures. The costs of the patients attributed to a specific ACO are then compared to the actual costs of the attributed beneficiaries’ digital twins. We believe this bottom-up analysis is more rigorous than other commonly used top-down approaches and model results have been systematically validated and published in leading medical journals.
2. RAF Capture Rate
RAF scores are determined in part by how carefully providers document care provided to their beneficiaries. To estimate how completely a given ACO documents care, HDAI matches each beneficiary to twins with similar RAF scores, demographics, and medical histories. We then compare any changes in RAF scores between ACOs over time. RAF scores that change more or less than twins may indicate important differences in coding practices.
SHARE
